Introduction
South Korea’s response to COVID-19 stands out because it flattened the epidemic curve quickly without closing businesses, issuing stay-at-home orders, or implementing many of the stricter measures adopted by other high-income countries. The country has shown early success across three phases of the epidemic preparedness and response framework: detection, containment, and treatment. From the outset, decision making in South Korea has been a collaboration between the government and the scientific community.
Detection: South Korea built hundreds of innovative, high-capacity screening clinics and worked closely with the private sector to ensure an adequate supply of tests. As the outbreak escalated, approximately 600 testing centers were established to screen people efficiently and outside of the health system, with testing capacity reaching 15,000 to 20,000 tests per day.
Containment: South Korea isolated infected patients, supported those in quarantine to increase compliance and, most importantly, traced contacts with unusual thoroughness. A workforce of hundreds of epidemiological intelligence officers was deployed for these tracing efforts and empowered to use a wide variety of data sources, including credit card transactions and closed-circuit television footage.
Treatment: The health system surged to meet demand, especially in Daegu, the site of a large cluster of infections. An additional 2,400 health workers were recruited in Daegu alone. Across the country, the government built temporary hospitals to increase capacity and addressed shortages of personal protective equipment (PPE) through centralized government purchasing.
South Korea’s strong enabling environment positioned the government to act quickly and effectively. After its flawed response to an outbreak of Middle East respiratory syndrome (MERS) in 2015, the government made several reforms to the health system to boost preparedness. In addition, a well-functioning national health insurance system, ample human resources and infrastructure, and constructive relationships with key institutions such as the president’s office, the Ministry of Health, and the Korean Centers for Disease Control and Prevention, allowed for an extraordinarily decisive response to the pandemic.
As South Korea transitions to reopening, its experiences may offer additional lessons about how to keep case numbers low without limiting activity.
Context
Since the 1960s, South Korea’s economy has grown at a remarkable pace. Its economy is currently the twelfth largest in the world1 and its health outcomes over the past 50 years have been commensurate with its economic progress. The country achieved universal health care coverage in 1989 (though a version of social health insurance has been in place since the 1970s), and the country transitioned to a single-payer system in 2004.2
South Korea’s health system is centered on hospital-based care. Compared to other high-income countries, the number of hospital beds per capita is much higher, at 12.3 beds per 1,000 population. This is over two times the average of Organization of Economic Cooperation and Development, or OECD, countries.3 Although some critics suggest that South Korea’s health system is over-indexed on hospitals—often sources of secondary or tertiary care—to the detriment of primary care, this increased capacity enabled hospitals to respond quickly to COVID-19 without sacrificing care for non-COVID-19 patients.4 Additionally, health care use in South Korea leads all other OECD countries at 16.6 consultations annually per capita.5
Despite its robust health system, South Korea struggled to respond appropriately to the 2015 outbreak of MERS, with nearly 17,000 suspected cases and 38 deaths. During the six months of that outbreak, Koreans lived in fear, and the government lost an estimated US$2.6 billion in tourism revenue while spending almost US$1 billion on diagnosis, treatment, and other response activities.
After MERS, the country made a series of policy changes to improve pandemic preparedness and response. When COVID-19 struck, the painful memory of MERS inspired an early, aggressive government response — and a willingness among people to wear masks, cooperate with contact tracers, and otherwise listen to public health officials. For example, wearing a mask in public spaces, already common because of air pollution, became a social norm early in the pandemic.6 A recent poll showed that more people adhered to public prevention protocols during the COVID-19 outbreak than during the MERS outbreak.7
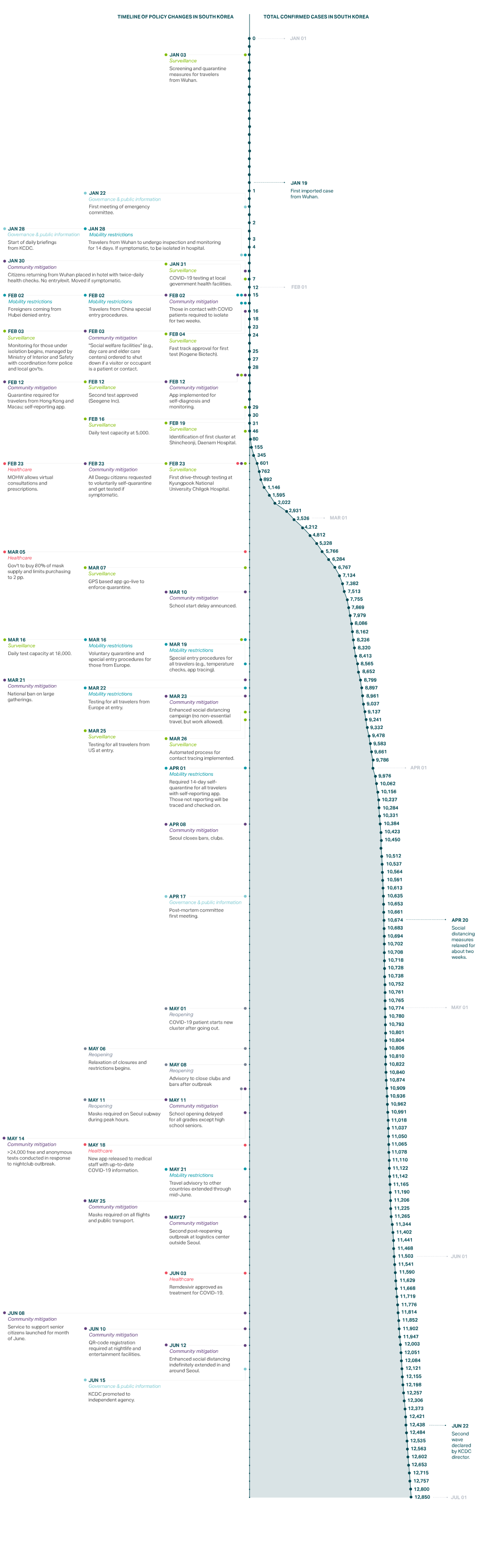
Outbreak Timeline
South Korea was one of the first countries to experience a COVID-19 outbreak, with its first case, imported from Wuhan, China, reported on January 20, 2020 (see Figure 1). The government established an emergency response committee within days of the case becoming known. The number of confirmed cases ranged from zero to two per day for the first month of the outbreak, until a cluster was identified in Daegu, a city of about 2.5 million. The cluster, which first appeared as 15 cases on February 19, was tied to the Shincheonji Church of Jesus. It originated from patient 31 who traveled around the cities of Daegu (including the church) and Seoul before her diagnosis.8 Thereafter, daily confirmed cases rose rapidly and reached a peak of 909 on February 29.
After this peak, the number of new cases fell rapidly in the following two weeks until it hovered below 200 daily confirmed cases by March 12. Daily cases steadily declined to nearly zero, although there was a minor resurgence in mid-May (about 30 cases per day) as the country started to reopen.
Detect
The Korean CDC received viral specimens from China to begin developing diagnostic tools even before the first case was confirmed in South Korea. As soon as the first case was reported, South Korea turned its focus toward preparing for large-scale testing. Many biotechnology companies sprang up in the years between MERS and COVID-19,9 enabling public-private partnerships to develop and scale up testing for SARS-CoV-2, the virus that causes COVID-19.
On January 27, 2020, a week after the first COVID-19 case, the Korean CDC directed private companies to produce a diagnostic reagent.10 Within two weeks of the first case, thousands of test kits were shipped daily, with the number reaching up to 100,000 kits per day in March.11 By April 24, 118 institutions were available to run diagnostic tests. Collectively, these institutions had the capacity to run an average of 15,000 tests (and up to 20,000) per day.
After expanding testing capacity, the focus then shifted toward screening. To prevent infected people from entering hospitals, for example, COVID-19 screening clinics were set up outside entrances. Those flagged by the screening were tested and told to return home and self-quarantine while they waited for results, while those deemed to be at low risk received a day entrance pass.
During the surge, health officials opened 600 screening centers using innovative approaches to increase capacity.12 For example, drive-through testing centers collected three times as many samples as conventional screening centers, while removing the need for negative pressure rooms that prevent contaminated air from escaping.13 Meanwhile, phone-booth style screen centers allowed health care workers to evaluate and test people without coming into direct contact with them. First, workers stood outside negative pressure booths wearing PPE. Eventually, they shifted to positive pressure booths, which minimized the need for PPE and thereby prevented fatigue.14 By late March, the country had performed over 300,000 tests in total, equal to a rate more than 40 times higher per capita than in the United States at that time.
Contain
The Korean government transformed public facilities and retreat centers owned by private corporations into temporary isolation wards. It did this for two reasons: to care for COVID-19 patients while preventing transmission within households, and to relieve hospitals of bed shortages. Health care workers regularly monitored and quarantined clinically stable patients who did not warrant inpatient treatment.15 In Daegu, the site of the first cluster, 15 community treatment centers, including several in dormitories for training institutes of private companies such as Samsung and LG, admitted 3,033 people between March 3 and March 26, 2020. Health professionals monitored the centers and patients reported their symptoms regularly by a smartphone application or by phone. The facilities were equipped with pulse oximeters, X-ray machines, and real-time reverse transcription polymerase chain reaction (RT-PCR) tests for SARS-CoV-2. Only 81 of 3,033 (2.67 percent) cases were transferred to a hospital for a higher level of care.16
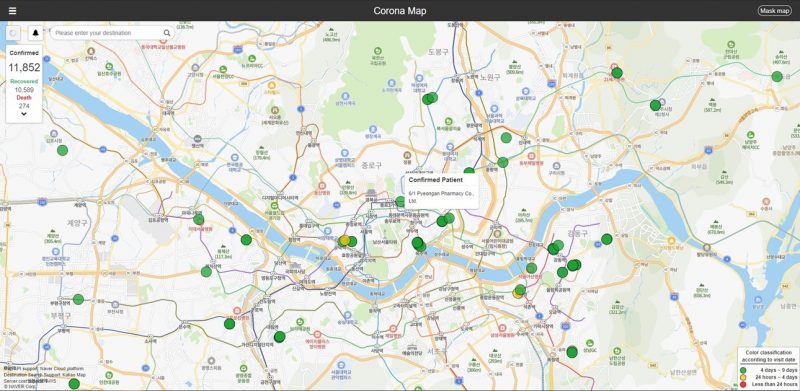
Example of South Korea’s private sector tool for contact tracing17
Meanwhile, staff at local public health centers closely monitored people who self-quarantined because they had been in contact with a confirmed case, had traveled internationally, or suspected they might be infected. A public health officer checked in with them twice daily and delivered food and toiletries.18
Summary of South Korea COVID-19 Epidemiological Survey Process19
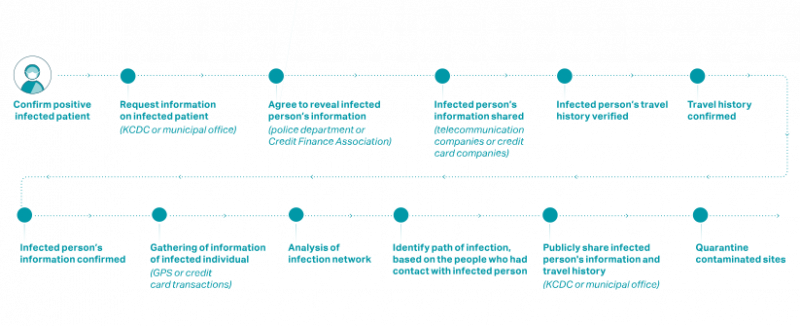
South Korea took an aggressive approach to contact tracing early in the outbreak. First, they scaled up their network of contact tracers. Second, they gave these workers access to different types of data, in addition to what they might be able to learn from the classic patient interview. Third, they used public communications to empower citizens to assist the health system with contact tracing.
South Korea expanded its usual workforce of Epidemic Intelligence Service (EIS) officers by quickly training staff at approximately 250 local public health centers, hiring 300 private epidemiologists, and leveraging staff at 11 nongovernmental organizations that train and support EIS officers. This multilevel approach was effective, with the veteran EIS officers conducting the more difficult investigations in large clusters and health facilities and temporary staff handling smaller clusters, including families. These efforts led to earlier case detection, kept the rate of new infections low, and potentially reduced crude fatality rates by preventing hospital overcrowding and infections among high-risk populations.20
Approach and Data Used to Monitor Contacts of COVID-19 Patients in South Korea21
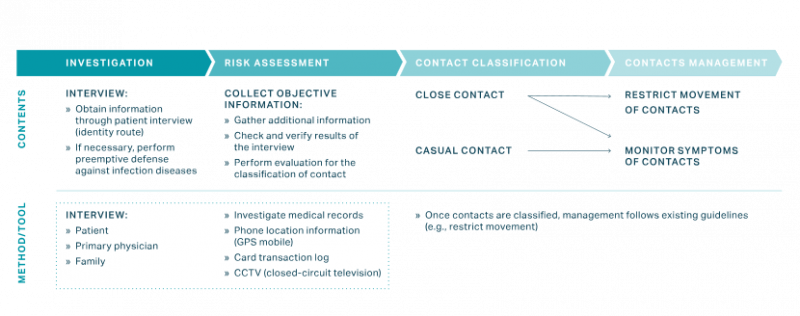
The work of the EIS officers was further facilitated by legal changes that followed the 2015 MERS outbreak. When necessary, the officers were permitted to draw on four major types of information in addition to patient and doctor interviews:
- Facility visits, including pharmacies and medical facilities
- Cellular GPS data from cell phones
- Credit card transaction logs
- Closed-circuit television
This information was combined with interviews and cross-checked with other data to identify contacts and take appropriate containment measures.22
Those identified as having had contact with a confirmed or suspected case were required to self-quarantine at home or in designated facilities for 14 days, as were travelers into the country. In late January, South Korea started requiring special entry procedures for travelers coming from Wuhan. Procedures initially included special entry lines and questionnaires, and later expanded to temperature checks, border-testing for all travelers, and mandatory quarantines that were monitored for 14 days. This policy of tracing and quarantining, rather than restricting entry, is in line with international health regulations, whereas border closures are not.23
South Korea made efficient use of technology to help ensure compliance with containment efforts by developing apps that collected relevant data, which eased the burden on EIS officers and made it possible for them to cope with the high volume of investigations. Patient trajectories were made public to enable citizens to track their own movements against those of suspected cases. Traveler information was shared with health facilities and pharmacies to facilitate prompt identification of cases and contacts.24
Treatment
South Korea defined the following seven groups as being at higher risk for severe illness from COVID-19: (1) people ages 65 and older; (2) people with underlying chronic conditions such as diabetes, chronic kidney, liver, or heart disease, and HIV; (3) people with blood cancer; (4) cancer patients receiving chemotherapy; (5) people taking one or more immunosuppressive medications; (6) pregnant women, extremely obese people, those undergoing dialysis, transplant recipients, and smokers; and (7) people with a blood oxygen saturation level below 90 percent. The country also ensured response readiness for these and other groups by running simulations of various outbreak conditions in hospitals before the start of the COVID-19 pandemic.
Securing requisite personnel and technology to rapidly surge capacity
During a shortage of hospital beds in the epicenter of Daegu, health officials developed a triage system using a Brief Severity Scoring System to classify patient illnesses as mild, moderate, severe, or critical. Mildly ill patients were sent to community treatment centers where they were closely monitored, moderately ill patients were sent to community hospitals, and severely or critically ill patients were hospitalized at tertiary hospitals equipped to provide intensive care.25
Using portable negative pressure devices, the government was able to rapidly expand the supply of temporary airborne infection isolation rooms. In Daegu, officials created about 400 additional negative pressure beds during the crisis.26
Daegu officials also recruited about 2,400 additional health care workers who were spread out among screening clinics, infectious disease hospitals, and community treatment centers. In addition, 327 physicians volunteered without pay to participate in the public health response, with 30 volunteering for the centralized COVID-19 response team and 260 volunteering for phone triage centers.
As with many cities around the world during the COVID-19 pandemic, Daegu faced a shortage of PPE, a critical issue that was escalated to the national government. Initially, the government limited the export of masks and penalized hoarding among retailers, but in mid-February, emergency measures doubled the production of masks in South Korea to an average of 10 million per day by March.
The government intervened in early March to purchase 80 percent of the mask supply from Korean manufacturers, fully ban exports, set a price limit on mask sales, and limit the number of masks sold weekly through retailers. Moreover, the government prioritized the distribution of masks to medical facilities. These interventions provided relief and averted further shortages, without forcing hospitals to issue policies about reusing PPE.27
Conclusion
We have many lessons to learn from South Korea’s experience with COVID-19, while also recognizing that the lessons may not be relevant to all countries.
South Korea, which is separated from China by North Korea, is effectively an island with respect to border travel and access. The population is highly urbanized, with over 80 percent living in urban areas.28 A rural, landlocked country is likely to face a different set of issues.
In fact, most cases in South Korea were clustered in more specific, confined areas than in China or other countries. Cases were often related to a small number of high-transmission events or locations, including megachurch services, other religious observances, a hobby sports group meeting, and workers in the tightly packed telecommunication center of a bank. As a result, meticulous contact tracing may have been easier than in other settings where cases spread through multiple smaller clusters and community transmission.29
Culturally and legally, South Korea is more tolerant of personal data-sharing, and its success has been heavily dependent on its ability to rapidly scale up technological solutions. Countries with less technology and where citizens do not have smartphones or are not as willing to share their data may experience difficulties adapting such strategies.
Despite these differences, many aspects of South Korea’s response are worthy of study, including its investments in preparedness, decisive and data-driven leadership, strategic clarity (a focus on testing and contact tracing), and willingness to be innovative. As of late May, South Korea is still determining how to best implement reopening procedures, laying out clear guidelines for how to maintain social distancing while getting back on the path to normal life. This is likely to be a bumpy road requiring more of the data-driven agility that has led to South Korea’s success so far. For example, just days after reopening, one man visiting five bars in Seoul led to an outbreak of more than 100 cases. After this exposure, health authorities tested and traced over 7,000 people.30
South Korea: Outbreak and Policy Action Timeline
In-depth explainers on Exemplar countries
This framework identified three countries which provide key success stories in addressing the pandemic: South Korea, Vietnam and Germany. In follow-up articles, in-country experts provide key insights into how these countries achieved this.